Antibiotic resistance is a silent pandemic because bacteria are evolving to beat the medicines we rely on, making infections harder to treat. This happens when antibiotics are misused in healthcare and agriculture, spreading resistant bacteria through water, air, and community contact. As bacteria share resistance genes, we face more dangerous, multi-drug resistant infections that increase illness, costs, and death rates. If you keep exploring, you’ll discover how global actions can help stop this growing threat.
Key Takeaways
- Antibiotic resistance develops from misuse in humans and agriculture, spreading resistant bacteria through the environment.
- Resistant bacteria produce enzymes, alter structures, or pump out antibiotics, making infections harder to treat.
- Horizontal gene transfer accelerates resistance spread among bacteria across communities and ecosystems.
- The rise of resistant strains leads to limited treatment options, longer illnesses, and increased mortality.
- Combating this silent pandemic requires global regulation, responsible prescribing, and reducing antibiotic misuse.
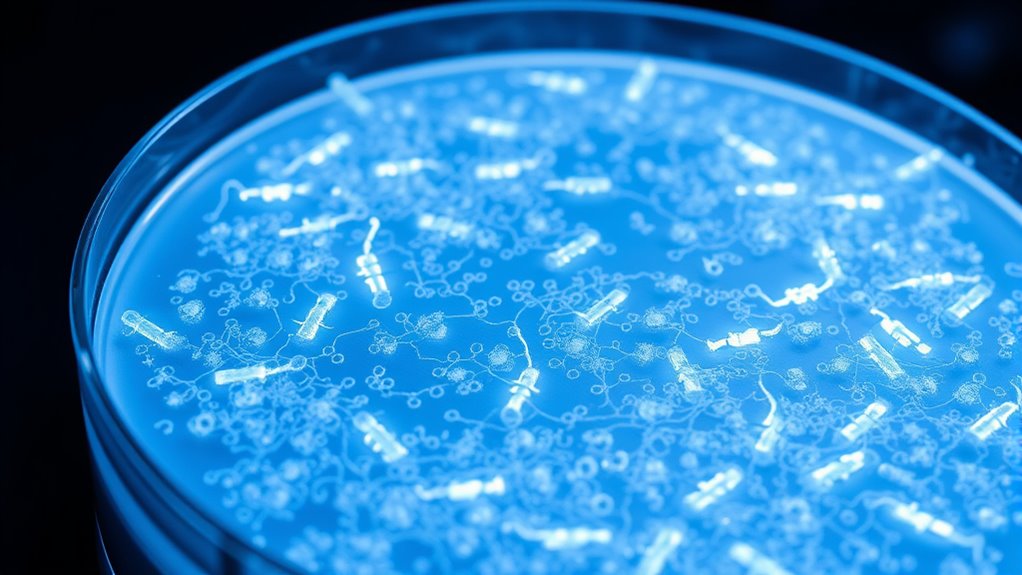
Have you ever wondered why some infections become harder to treat? The answer lies in the growing threat of antibiotic resistance, a silent pandemic spreading across the globe. One of the key drivers behind this crisis is the misuse in agriculture. Farmers often use antibiotics to promote growth and prevent disease in healthy animals, thinking it boosts productivity. However, this practice exposes bacteria to antibiotics unnecessarily, giving them opportunities to adapt and develop resistance. When these resistant bacteria make their way into the environment through manure or runoff, they can transfer resistance genes to other bacteria, including those that infect humans. This widespread misuse in agriculture creates a perfect storm for resistance to flourish. The resistance mechanisms bacteria employ are diverse and continually evolving, making it a significant challenge to combat resistant infections.
Misuse of antibiotics in agriculture fuels the rise of resistant bacteria and threatens global health.
Understanding resistance mechanisms is essential to grasping how bacteria overcome antibiotics. Bacteria aren’t passive; they have several tricks up their sleeves. Some produce enzymes that deactivate antibiotics, rendering them ineffective. Others alter the structure of their cell walls or change binding sites so antibiotics can’t latch onto them. Some bacteria can pump antibiotics out of their cells before they do damage. These are all resistance mechanisms that bacteria evolve in response to antibiotic exposure. When antibiotics are overused or misused, bacteria are constantly challenged, and only those with resistance mechanisms survive and multiply. Over time, this leads to the proliferation of resistant strains that are much harder to kill.
The problem intensifies because resistance isn’t confined to hospitals or farms; it spreads through communities, water sources, and air. When resistant bacteria survive antibiotic treatments, they can share their resistance genes with other bacteria via horizontal gene transfer. This genetic exchange accelerates the development of multi-drug resistant bacteria, making infections less responsive to standard treatments. As resistance spreads, doctors find themselves with fewer options, leading to longer illnesses, higher medical costs, and increased mortality rates.
You might think that antibiotics are a quick fix, but their misuse—whether in agriculture, medicine, or everyday use—fuels this resistance. It’s essential to understand that bacteria are constantly evolving, and their resistance mechanisms are becoming more sophisticated. To combat this silent pandemic, we need stricter regulations on antibiotic use, particularly in agriculture, and a global effort to promote responsible prescribing practices. Only then can we slow the rise of resistant bacteria and preserve the effectiveness of antibiotics for future generations.
Frequently Asked Questions
How Quickly Is Antibiotic Resistance Spreading Globally?
You might not realize how fast antibiotic resistance spreads globally. Due to antibiotic misuse, bacteria develop resistance quickly, and resistance gene transfer accelerates this process across different species and regions. This rapid dissemination is fueled by overprescribing and improper use, making infections harder to treat worldwide. Staying aware of these factors helps you understand the urgency of combating resistance and reducing misuse to slow its spread.
Are There New Antibiotics Being Developed to Combat Resistance?
While resistance spreads rapidly, new antibiotics are still in development. You’ll find innovative efforts in novel drug discovery, aiming to outpace resistance. Researchers also improve resistance monitoring techniques, helping identify threats early. Although progress is slow, these advancements give hope. You can support these efforts by staying informed and advocating for sustained investment in research, ensuring we develop effective treatments before resistance renders current antibiotics obsolete.
What Are the Most Common Drug-Resistant Bacteria?
You should know that the most common drug-resistant bacteria, or superbugs, emerge through various resistance mechanisms, making infections harder to treat. These superbugs, like MRSA, resistant gram-negative bacteria, and Clostridioides difficile, develop resistance by altering drug targets or pumping out antibiotics. Understanding their emergence helps you recognize the importance of proper antibiotic use and infection control to prevent their spread and combat rising resistance.
How Does Antibiotic Resistance Affect Vulnerable Populations?
You should know that vulnerable populations, like the elderly and those with weakened immune systems, face a 60% higher risk of complications from resistant infections. Antibiotic resistance worsens health disparities, making it harder for these groups to access effective treatments. As a result, infections last longer, hospital stays increase, and mortality rates rise, highlighting the urgent need to protect and support vulnerable populations against this growing threat.
Can Alternative Therapies Replace Antibiotics Entirely?
You might wonder if alternative therapies can fully replace antibiotics. While natural remedies and herbal treatments can support your health and help fight some infections, they can’t replace antibiotics for serious bacterial illnesses. These alternatives may boost your immune system or reduce symptoms, but antibiotics remain essential for effectively treating severe infections. It’s important to consult healthcare professionals before replacing antibiotics with any alternative therapies.
Conclusion
So, here you are, thinking antibiotics will always save you. Ironically, your reliance on them may be what’s causing their demise. As bacteria become resistant, those life-saving drugs lose their power, leaving you more vulnerable than ever. It’s a silent pandemic you helped create—by ignoring the warning signs and overusing antibiotics. Maybe, just maybe, the real threat isn’t bacteria itself, but our own complacency. The irony is, your comfort today could be your crisis tomorrow.










